Purpose
To provide challenging MEP identification examples. More general information on how to identify MEPs in EMG traces and how to determine MEP status can be found in the Simple MEP Identification module.
Examples of challenging MEP identification
Here are some examples that classify patients as MEP+ or MEP- based on their EMG traces that are complicated by delayed latency and/or the presence of biological and non-biological noise (see EMG Technique page for more information). For example, if the patient is performing bilateral facilitation then you will need to determine MEP status in the presence of intentional muscle activation.
Traces should be considered representative of all EMG traces for the patient.
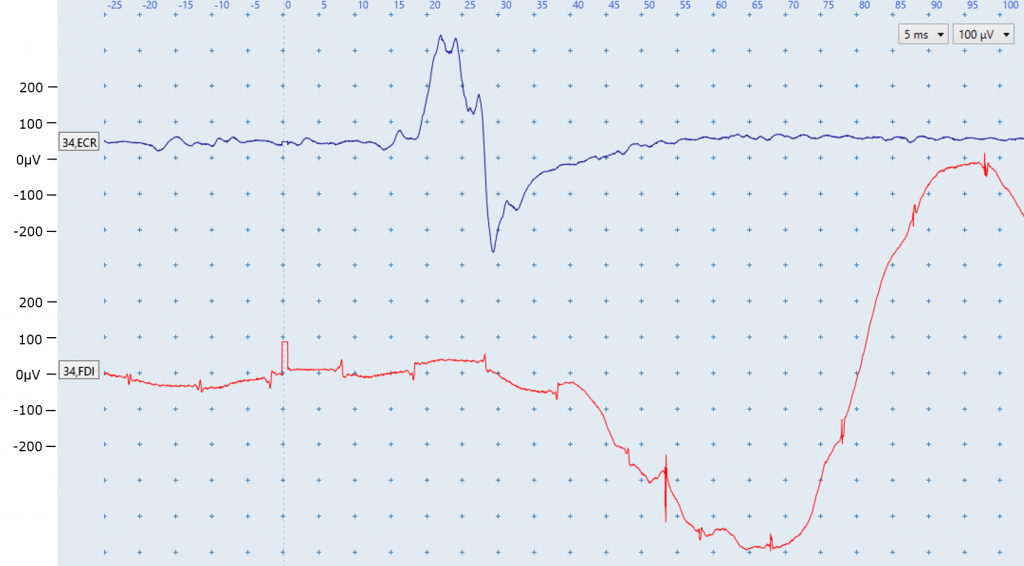
A: Patient (5ft 5”) performing active bilateral facilitation, 100% MSO
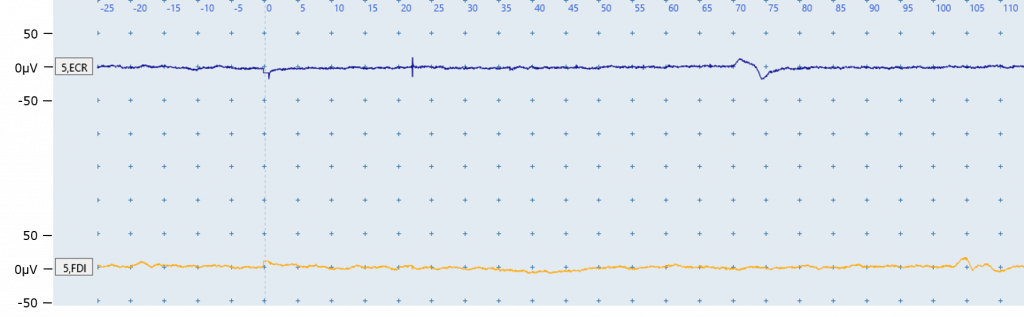
A: No muscle activity can be detected in the EMG despite patient A’s best efforts to activate both upper limbs during bilateral facilitation. A MEP-like response is identified in the ECR EMG trace, but it occurs very late at ~70 ms. No MEP is identified in the FDI trace. If 4 other scalp locations had been stimulated prior to this figure with no MEPs present then patient A can be classified as MEP-.
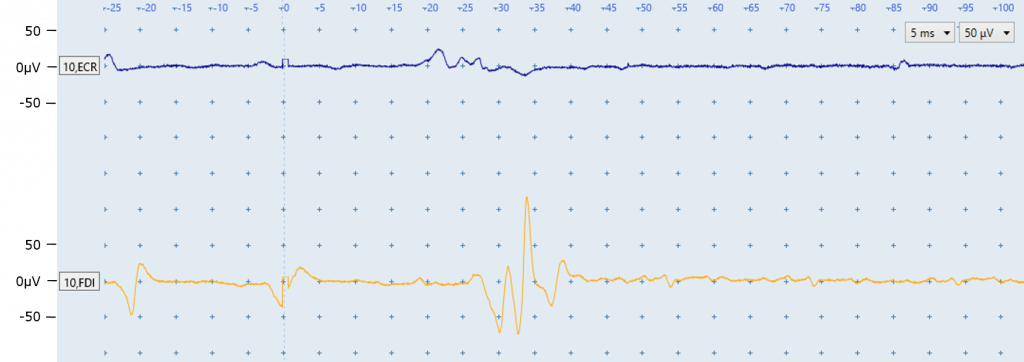
B: Patient (5ft 8”) performing active bilateral facilitation, 100% MSO
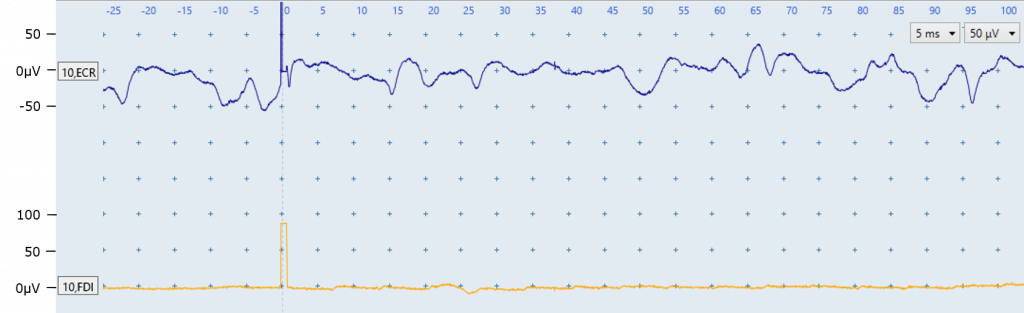
B: This patient had no MEPs at 100% MSO while at rest the and is therefore attempting active bilateral facilitation to increase the likelihood of eliciting a MEP. Evidence of muscle activation due to the bilateral facilitation is seen in the ECR trace so this noise should not be troubleshooted. No MEP is identified in the ECR post-trigger trace. No MEP is identified in the FDI EMG trace. If 4 other scalp locations had been stimulated prior to this figure also with no MEPs present then patient B can be classified as MEP-.
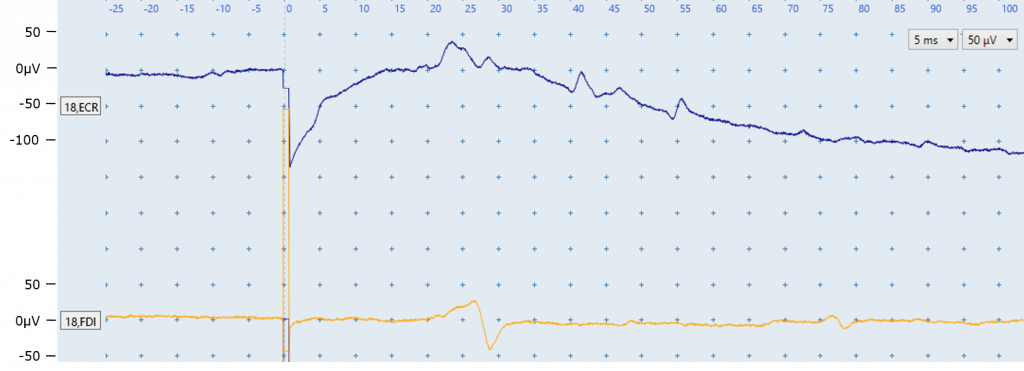
C: Patient (5ft 7”) performing active bilateral facilitation, 100% MSO
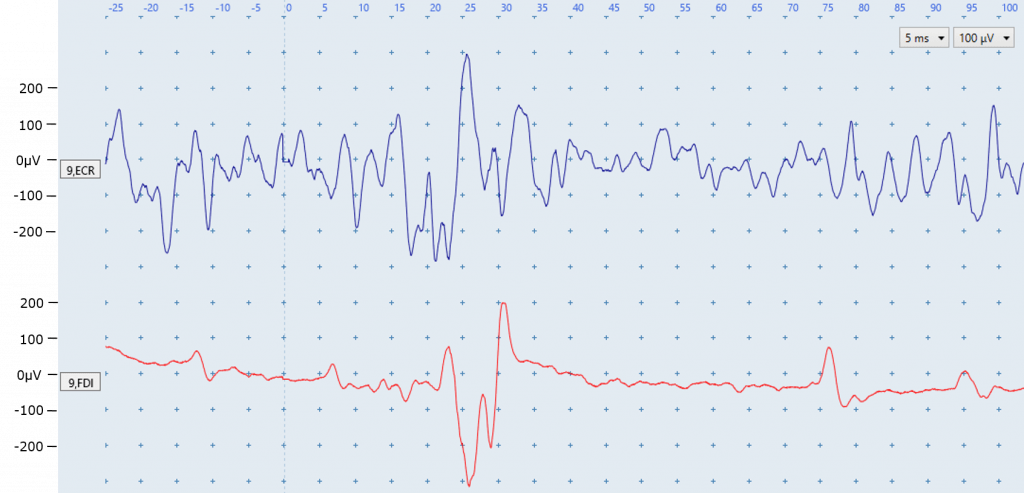
C: This patient had no MEPs at 100% MSO while at rest and is attempting active bilateral facilitation to increase the likelihood of eliciting a MEP. Evidence of intentional muscle activation due to voluntary contraction is seen in both traces. A clear MEP is identified in the FDI trace at the appropriate latency (~20ms). There is no clear ECR MEP. This patient can be classified as MEP+, based on the presence of FDI MEPs.
D: Patient (5ft 6”) performing active bilateral facilitation, 100% MSO
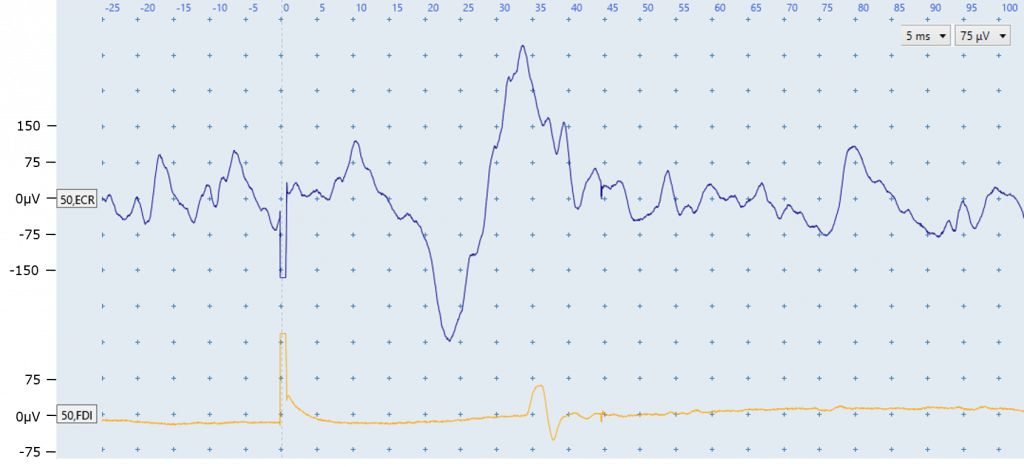
D: This patient had no MEPs at 100% MSO while at rest and is attempting active bilateral facilitation to increase the likelihood of eliciting a MEP. Evidence of intentional muscle activation due to voluntary contraction is seen in in the ECR EMG trace before stimulation. A MEP is identified in the ECR EMG trace at an appropriate latency of ~20ms, with EMG activity returning to that seen pre-trigger soon after. There is an FDI MEP that is just slightly after the typical expected latency. This patient can be classified as MEP+, based on the presence of ECR MEPs.
If ECR MEPs were absent and FDI MEPs were consistently present (most EMG traces) at about this same latency (~ 34 ms) the patient may be classified as MEP+. However it would be important to check MEP size and shape across all traces to rule out motor unit firing.
E: Patient (5ft 6”) at rest, 70% MSO
E: The FDI EMG trace (bottom) is clearly contaminated by electrical noise. However, a MEP is identifiable in the ECR EMG trace at an appropriate latency. This patient can be classified as MEP+, based on the presence of ECR MEPs. The EMG set-up for FDI should be checked for issues such as a loose cable, poor electrode conduction due to lack of contact with skin, or a faulty electrode.
F: Patient (5ft 9”) at rest, 70% MSO
F: A MEP is clearly identifiable in the FDI EMG trace at an appropriate latency. A smaller MEP is identified in the ECR EMG trace at an appropriate latency. The other fluctuations seen in both muscle EMG traces are not MEPs. These are motor units firing sporadically. They can be identified due to their consistent size and shape, and appearance at latencies which do not correspond with the expected latency for ECR or FDI. In both traces the motor units also fire prior to delivery of the TMS stimulus. This patient can be classified as MEP+, based on the presence of ECR or FDI MEPs.
G: Patient (5ft 7”) at rest, 80% MSO
G: It is difficult to determine whether there is a MEP present in the ECR EMG trace, due to the elongated stimulus artefact and downward drifting signal. The EMG set-up for ECR should be checked for issues such as a loose cable, poor electrode conduction due to lack of contact with skin, or a faulty electrode. A response is identified in the FDI EMG trace at an appropriate latency for a MEP. In addition, a similar-shaped small response is identified later in the FDI trace (~ 75 ms) which may be a motor unit firing. Before classifying based on information from the FDI trace alone, it would be good to see whether other traces also have a response at 20 ms.
H: Patient (5ft 8”) at rest, 50% MSO
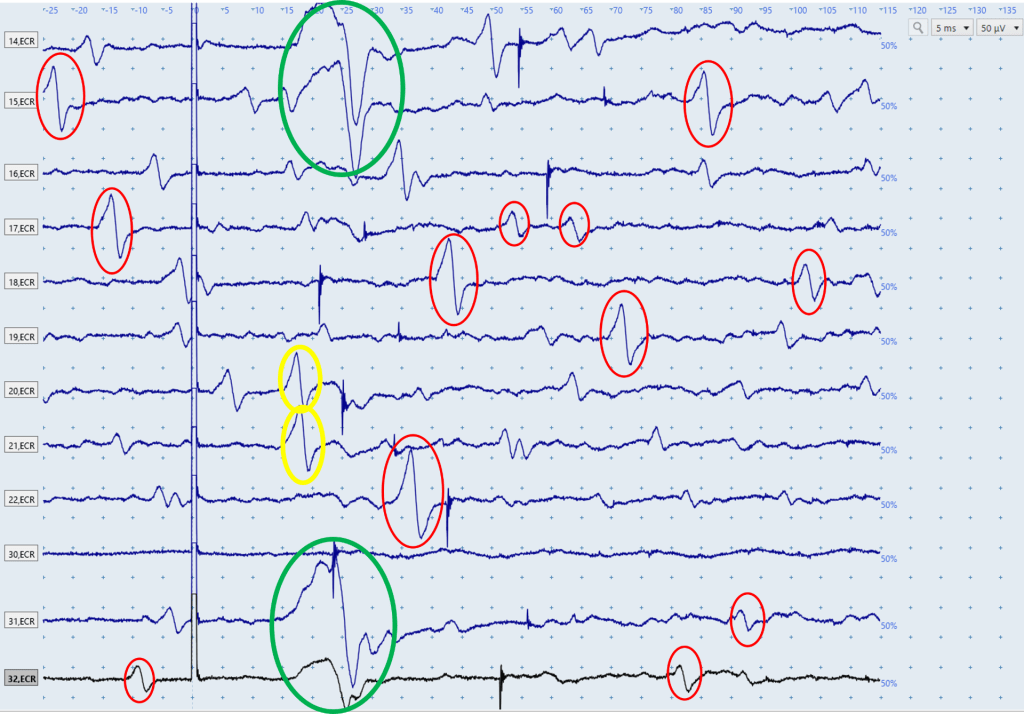
H: The above figure displays a series of ECR EMG traces, each of which is the result of a single stimulation. An ECR MEP is present in the first two and last two traces, and these can be seen in the green circles. You can be confident these are MEPs because their shape is similar and they all have a latency of ~18 ms, which is within the expected window for ECR MEPs. Throughout the traces there are a high number of motor units firing, some of which are highlighted in red circles. Although these responses vary in size, their consistent shape and appearance at latencies that don’t correspond to the expected ECR MEP latencies indicates they are motor units firing sporadically. There are many other motor units firing in these traces that haven’t been circled. The two responses in yellow are within the expected window for ECR MEP latencies, however the fact their shape is so similar to the motor units firing, and so dissimilar to the MEPs present in the first and last two traces, indicates they are likely also motor units firing sporadically.
I: Patient (6ft 1”) at rest, 80% MSO
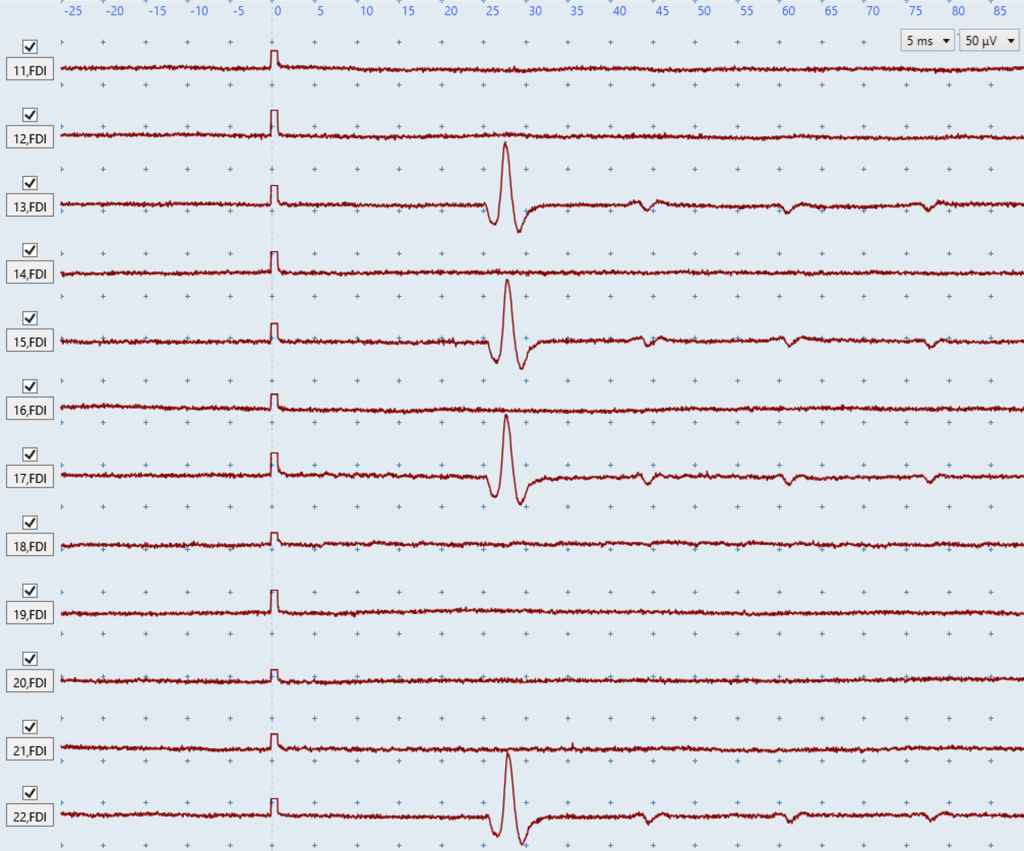
I: The above image shows a series of FDI traces, and 4 of them have deflections at ~25 ms. The latency, shape, and amplitude of these deflections is nearly identical which suggests they may be motor units firing. However, these are likely to be MEPs rather than motor units firing for several reasons. First, they appear at ~25ms which is within the expected latency for FDI MEPs. Second, if the large deflections at ~25 ms were motor units we’d expect to see deflections of similar shape and amplitude appear at different latencies between traces but they are all consistent at ~25 ms. The small deflections at ~42 ms, ~60 ms, and ~75 ms are likely to be motor units though given their latencies. In order to be certain the deflections at ~25 ms were MEPs it’d be useful to reposition the participant’s hand and arm and see if the same responses appear, as well as increase the stimulus intensity by 10% to see if the shape or amplitude of the responses changes.
J: Patient (6ft 6”) at rest, 50% MSO
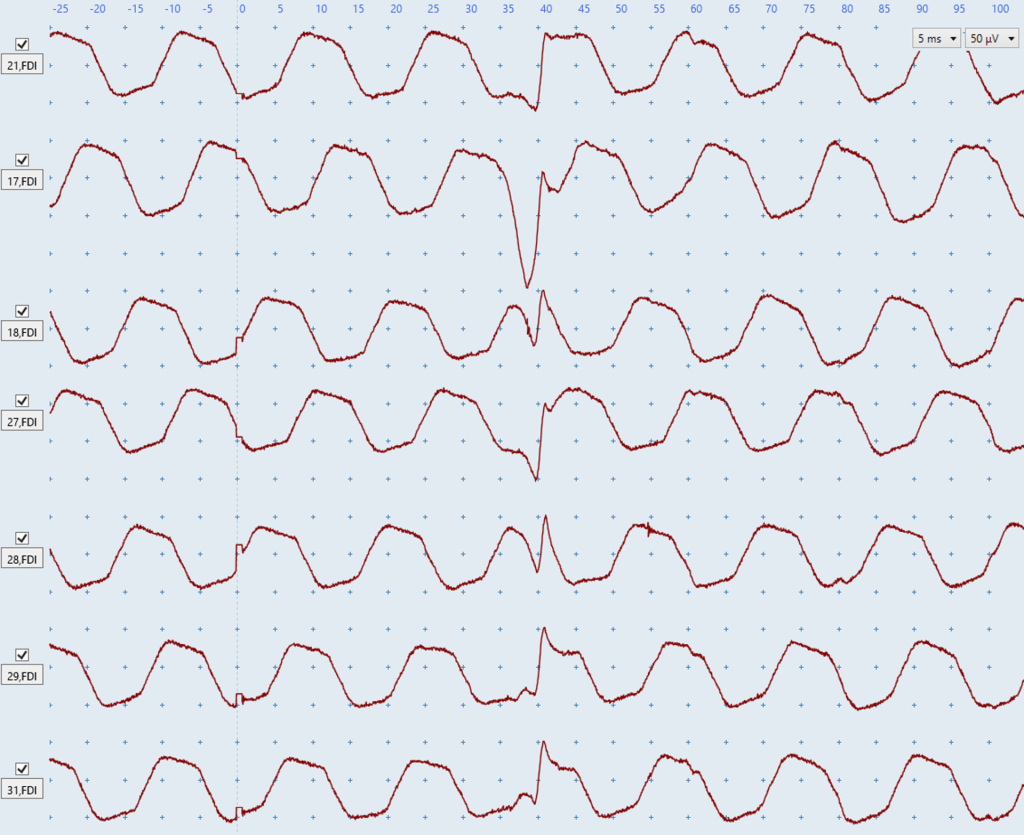
J: The above figure shows a series of FDI traces with severe electrical noise present. Looking at any of these traces individually, especially traces such as 21 and 29, may lead you to think no MEPs are present. However it’s only once viewing all these traces together you can see the very consistent nature of the deflections at ~38 ms which indicates this patient is MEP+. Even the upwards deflection in trace 21 at ~38ms is sharper than the surrounding electrical noise. Although 38 ms is reasonably late compared to the expected FDI latency range of ~20-30 ms, MEP latency can be delayed in stroke and depends on the person’s height so this is not an unreasonable latency.
MEPs typically become larger with increasing stimulus intensity so a good idea for subject J would be to increase the stimulus intensity another 10% to see if the MEPs become larger and more obvious amongst the electrical noise.
Quiz
Click here for a quiz to assess your learning on Challenging MEP Identification.
Once the practice quiz has been completed with at least 70% correct you will be emailed a link to a short survey to complete. This survey asks about your confidence and experience with TMS now that you have completed the self-directed TMS training modules.
Once you complete the TMS Post Self-Directed Training survey you will be emailed a link to the final Challenging MEP Identification quiz. If you pass the final quiz with at least 80% correct you will be emailed a certificate of completion for the Challenging MEP Identification module. There is no limit to the number of attempts for the practice or final quiz.
Please email verify.study.tms@gmail.com if you have any questions or comments.
